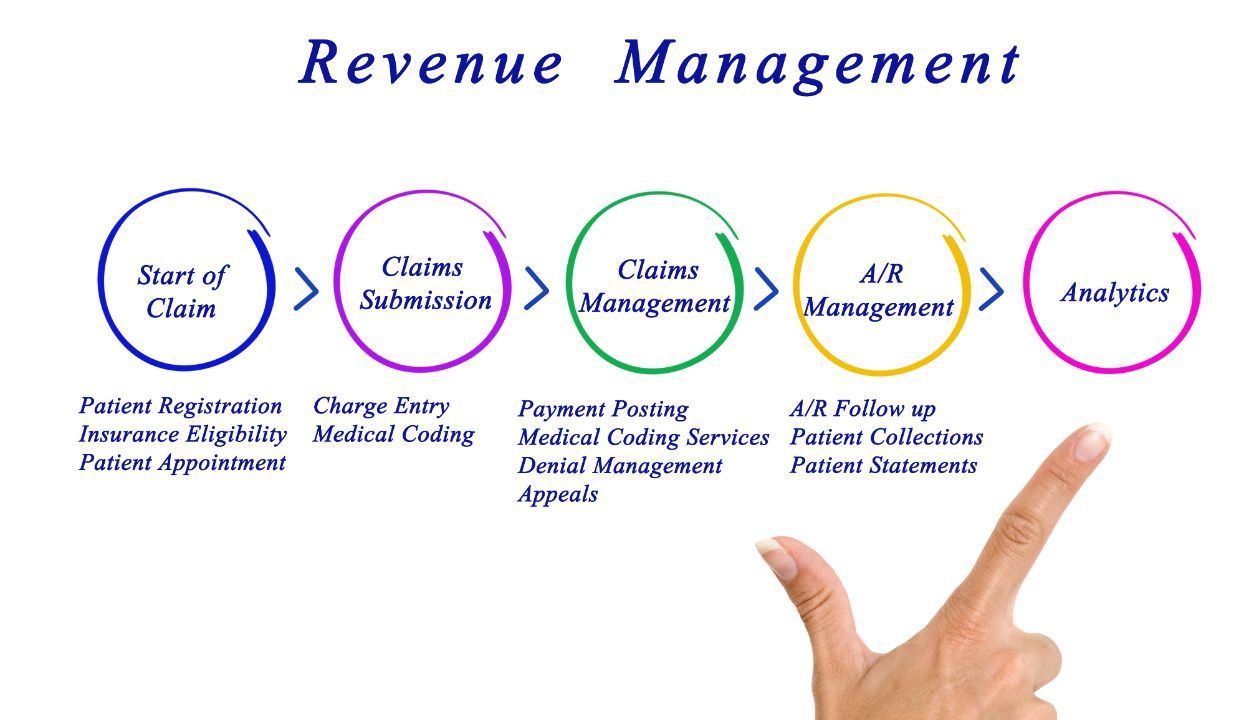
The healthcare industry will continue to face increasing regulatory complexities, operational challenges, and financial pressures. Revenue cycle management (RCM) is a critical function that often bears the brunt of these challenges. Manual, error-prone processes, coupled with rising patient volumes, can lead to delayed reimbursements, increased costs, and decreased patient satisfaction.
Robotic process automation (RPA) is the emerging technology that offers a transformative solution to these persistent problems.
By automating repetitive, rule-based tasks, RPA can significantly enhance efficiency, accuracy, and cost-effectiveness across the entire RCM spectrum. From streamlining patient intake to accelerating claims processing, there are significant financial benefits to incorporating RPA in your healthcare organization.
In this article, we explore the specific revenue cycle processes that stand to benefit the most from RPA implementation. We’ll cover how RPA can address common challenges, improve operational efficiency, and drive substantial financial returns.
Advantages of RPA in RCM
There are quite a few key advantages of incorporating robotic process automation in your revenue cycle management operation.
- Improved Efficiency: RPA can dramatically accelerate RCM processes by automating time-consuming tasks such as data entry, claims submission, and eligibility verification. This frees up staff to focus on higher-value activities like patient care and complex claim resolution.
- Enhanced Accuracy: Manual data entry is a leading cause of errors in managing revenue cycle at a healthcare practice. RPA eliminates this risk by automating data transfer and validation, ensuring patient data accuracy and integrity.
- Cost Reduction: By automating repetitive tasks, RPA can lead to significant cost savings for healthcare practices through reduced labor costs, lower error rates, and faster claim processing.
- Compliance Adherence: RPA can help healthcare organizations maintain compliance with complex regulations by automating compliance-related tasks such as audit preparation and reporting.
- Increased Patient Satisfaction: Streamlined RCM processes, enabled by RPA, can result in faster appointment scheduling, reduced wait times, and improved billing accuracy, leading to increased patient satisfaction.
In the following sections, we’ll outline specific RCM processes that are prime candidates for RPA implementation and provide real-world examples of successful RPA deployments in healthcare.
Key Revenue Cycle Management Processes that Benefit From RPA
Most every step of the RCM process can benefit from robotic process automation, but some areas have a more significant impact than others on both cost savings and revenue enhancement.
Embracing robotic process automation empowers staff to focus on higher-value tasks. By automating these middle and back-end RCM processes, healthcare organizations can significantly improve efficiency, accuracy, and financial performance.
Middle and Back-End RCM Processes
Charge Capture: Accurate charge capture is critical for complete and compliant claims. RPA can automate charge capture by extracting patient information, procedures performed, and associated charges from EHRs. RPA creates standardized charge codes and appends them to patient accounts.
This automation improves charge capture accuracy, reduces lost charges, and enhances overall claim reimbursement.
Claims Submission: Accurate and timely claim submission is crucial for revenue generation. RPA can significantly enhance this process by automating data extraction from EHRs and patient records.
RPA validates information and electronically submit claims to payers.
This automation reduces manual errors, accelerates claim processing, and improves claim acceptance rates.
Payment Posting: Payment posting is a time-consuming process prone to errors. RPA can automate this task by extracting payment information from remittance invoices, reconciling payments with patient accounts, and posting them to the appropriate accounts.
This automation improves cash flow, reduces manual errors, and provides real-time financial insights.
Denial Management: Claim denials can significantly impact revenue. RPA can streamline denial management by automatically categorizing denials based on reasons, extracting relevant information, and routing them to appropriate departments for resolution.
This automation reduces manual effort, accelerates denial resolution, and improves claim reimbursement rates. Dive deeper into how to manage claim denials.
AR Follow-up: Effective AR follow-up is essential for improving collections. RPA can automate routine follow-up tasks by sending automated reminders, generating patient statements, and escalating overdue accounts.
This automation improves collection efficiency, reduces write-offs, and enhances cash flow.
Unislink: Your Partner in RPA for Practice Success
Unislink can be a valuable partner in helping healthcare practices harness the power of RPA to transform their revenue cycle management (RCM) operations. With a deep understanding of the healthcare industry and expertise in RPA implementation, Unislink can provide tailored solutions to address specific RCM challenges.
Key benefits of partnering with Unislink
- Comprehensive RPA Assessment: Unislink can conduct a thorough evaluation of your RCM processes to identify areas where RPA can deliver the greatest impact.
- Customized RPA Solutions: By understanding your unique practice needs, Unislink can develop and implement RPA solutions that align with your goals.
- Integration Expertise: Unislink can seamlessly integrate RPA with your existing EHR and practice management systems, ensuring a smooth transition.
- Ongoing Support and Optimization: Unislink provides ongoing support to monitor RPA performance and optimize processes for maximum efficiency.
Contact us today to learn more about how Unislink’s expertise can help healthcare practices streamline RCM operations, reduce costs, improve accuracy, and enhance patient satisfaction.