Billing & Revenue Cycle Solutions for
Dermatology Practices
In a fast-paced dermatology practice, you are balancing a high volume of patients across medical, surgical, and aesthetic disciplines. The financial challenges are unique and constant: navigating the “global period” for biopsies and excisions, managing complex modifiers for same-day procedures and office visits, and ensuring accurate billing for high-cost biologics and pathology services.
These administrative complexities can slow your workflow and lead to significant revenue leakage if not managed with precision.
UnisLink provides a dedicated and professional approach to revenue cycle management (RCM), designed to streamline your operations and secure your practice’s financial health. We handle the intricacies of dermatology medical billing so your team can focus on what they do best—providing expert skin care.
Read our blog article
“Transition from ICD-10 to ICD-11: A Fundamental Shift for U.S. Healthcare Practices”
UnisLink – Tailored Specifically for Dermatology Groups
Your Financial Health is Our Priority
UnisLink is more than just a medical billing service—we are an extension of your practice. We combine deep industry expertise in Dermatology RCM with powerful technology to tackle these challenges head-on, so you can focus on what matters most: your patients’ health and outcomes.
Our Dermatology RCM solutions address the top challenges for your specialty:
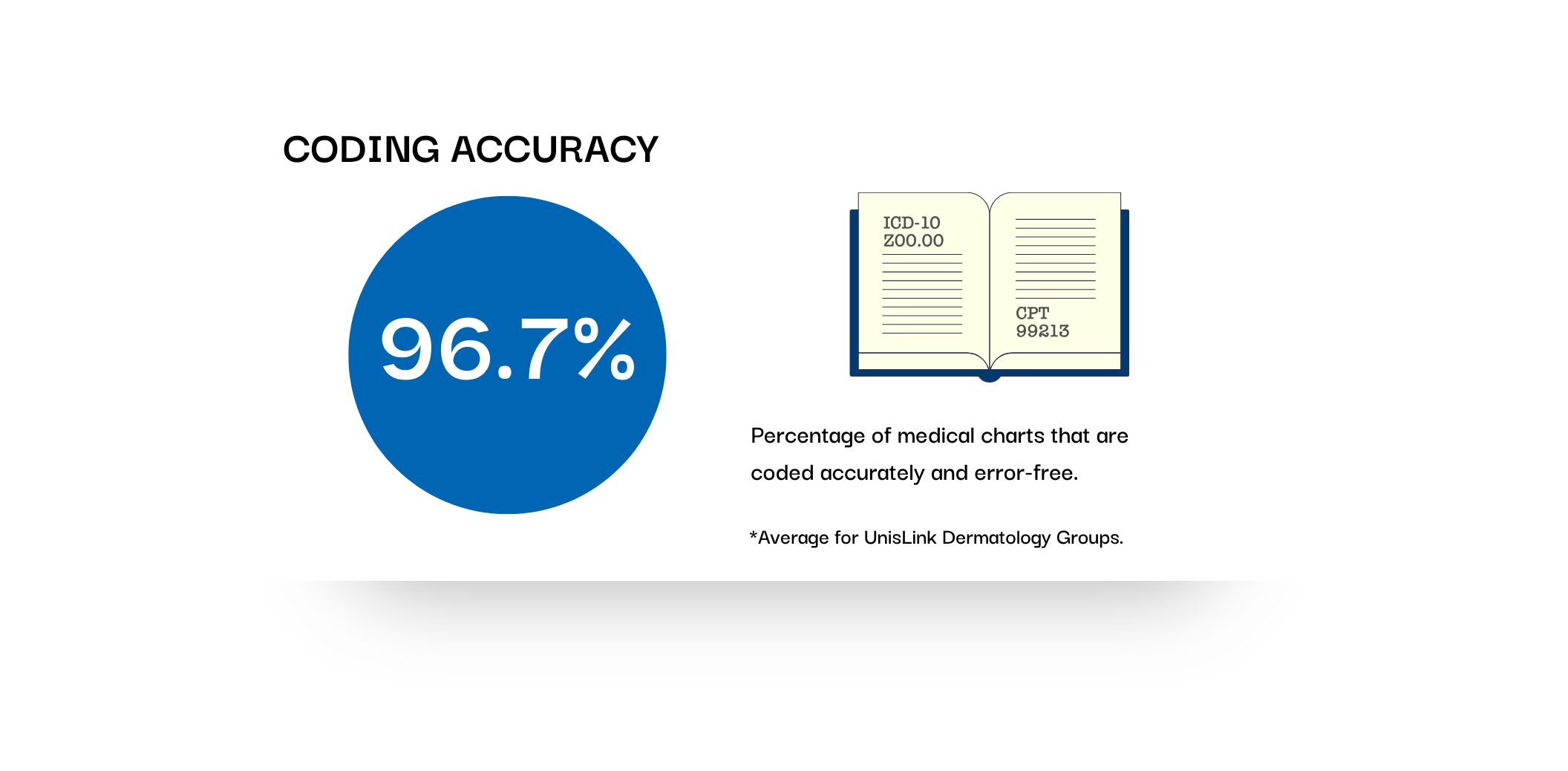
- The Modifier -25 & Global Period Trap Billing for an office visit and a procedure (like a biopsy or cryotherapy) on the same day is often a target for payer denials. UnisLink’s certified professional coders and AI technology ensure the correct application of modifiers and adherence to global surgical periods, delivering 95% accuracy to protect your revenue from “unbundling” rejections.
- High-Volume Procedural & Pathology Billing With dozens of minor procedures performed daily, missed charges can add up to thousands in lost revenue. We integrate directly within your existing EHR to ensure every excision, destruction, and pathology component is captured and billed with the specific morphology and site requirements demanded by payers.
- Staffing Shortages & Aesthetic Revenue Separation Finding billers who understand the nuances of dermatology is difficult. UnisLink provides an “instant back-office” of specialty-focused talent, while our AI-driven patient collections systems clearly separate clinical balances from cosmetic/self-pay services, making it easier for patients to pay and lowering your Total Cost to Collect.
- Lack of Specialized Financial Insight Most billing systems don’t provide the granularity needed to track the profitability of specific lasers, Mohs labs, or aesthetic lines. Our Engage Analytics™ platform provides real-time, transparent access to your data, allowing you to see exactly which service lines are driving your growth and which require optimization.
Experience the UnisLink Difference.
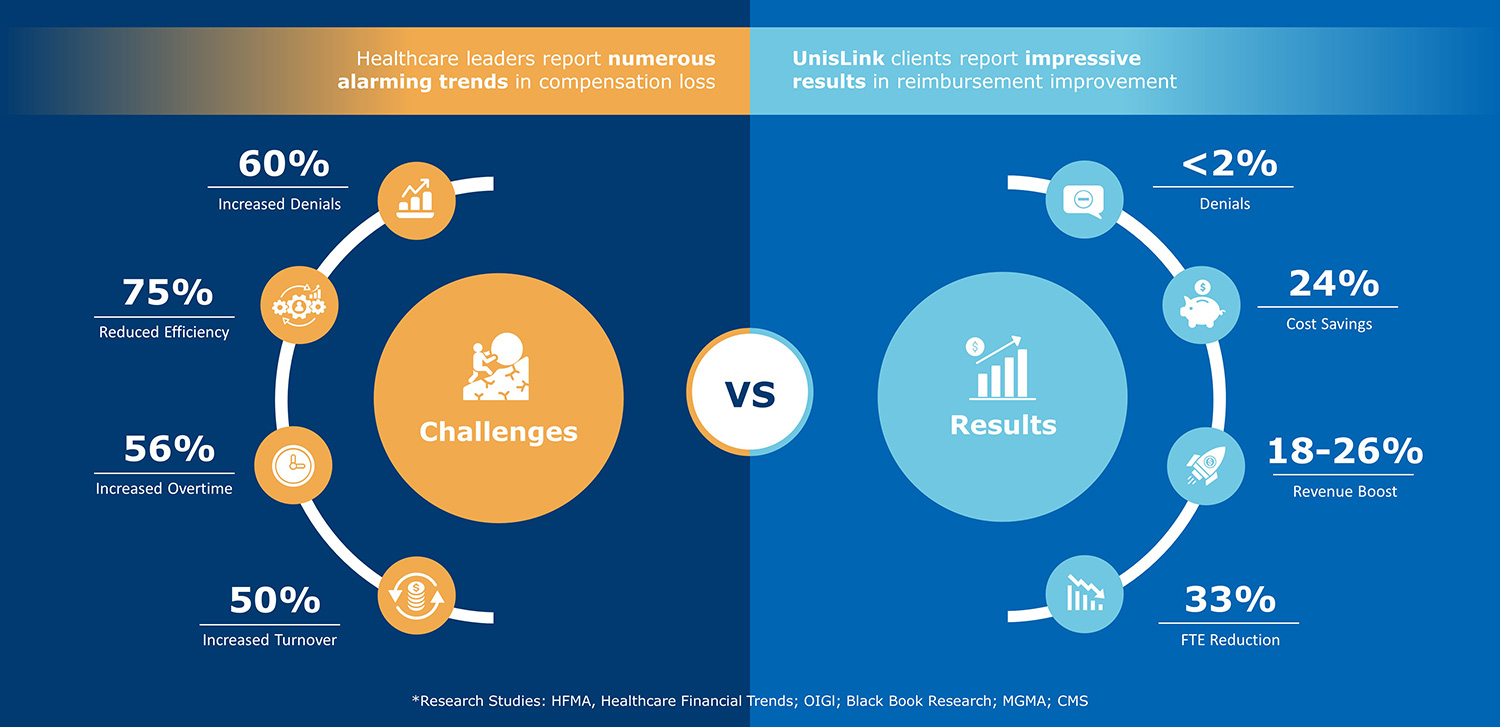
Other companies often present solutions without truly understanding your problems. UnisLink ensures its medical billing services target exactly what hospitalists need to increase the KPIs that really matter.
The result? More revenue.
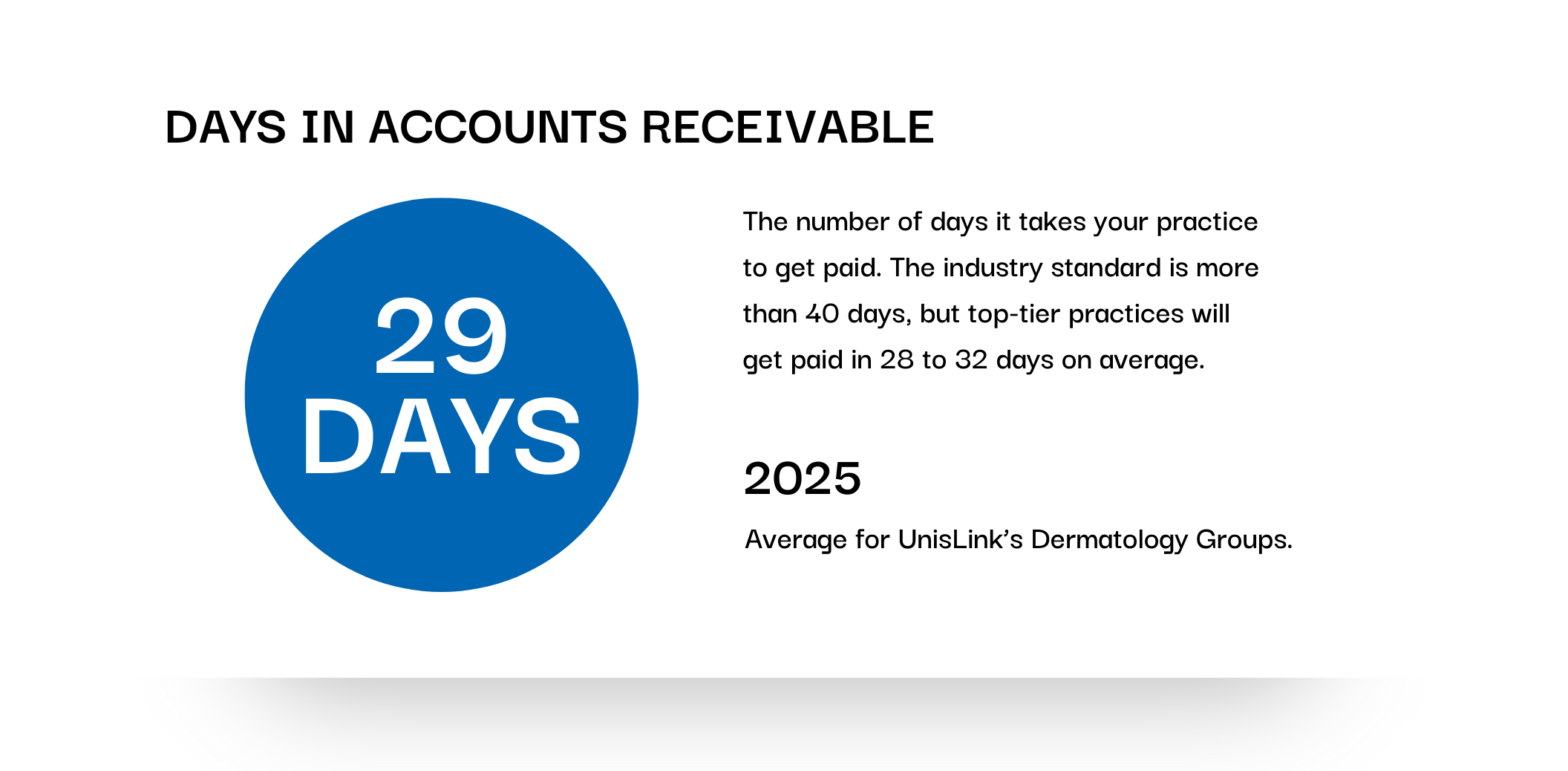
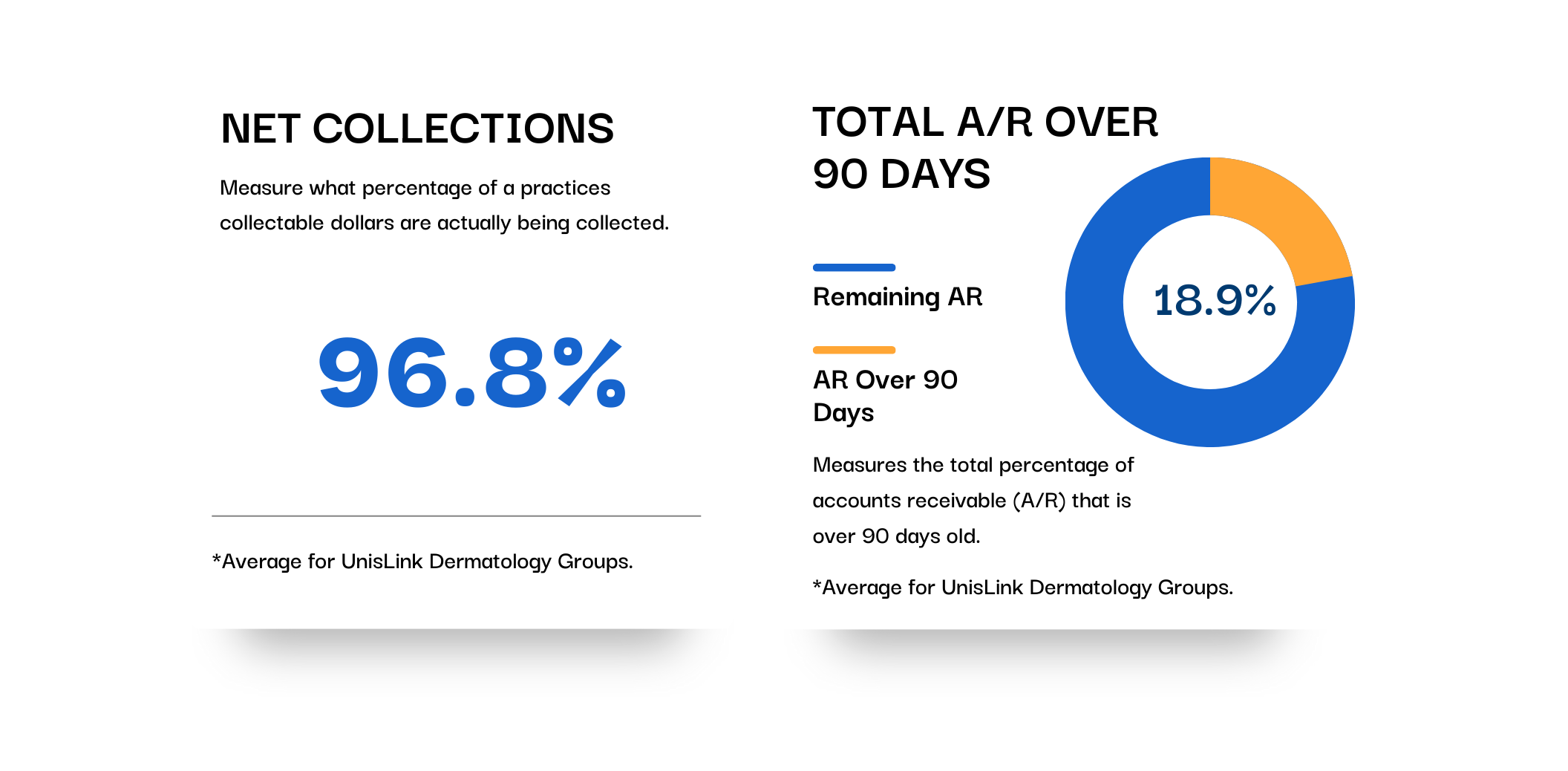
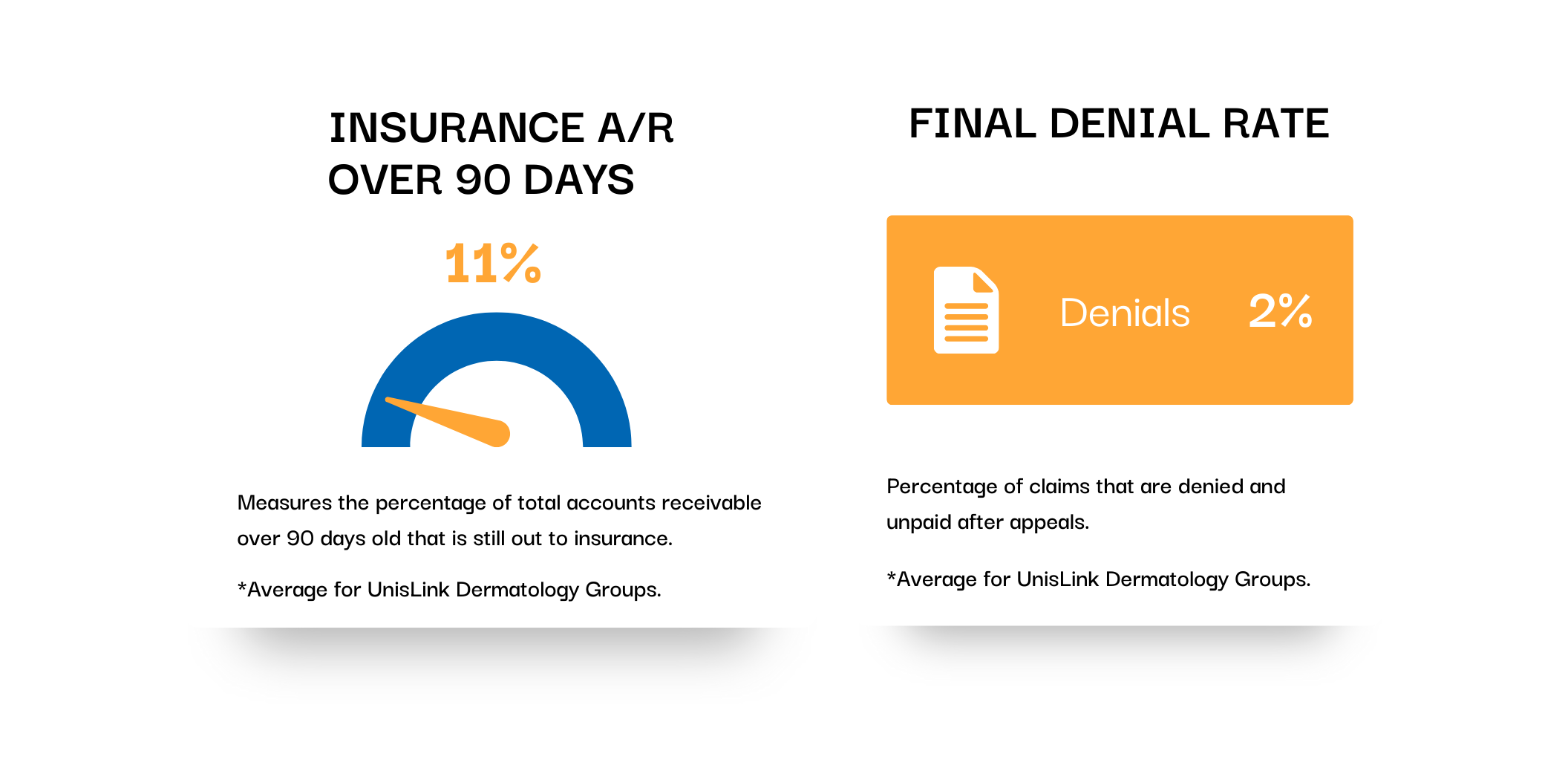
How much revenue improvement can you expect?
Improve your claim submission accuracy and increase cash flow by uncovering leaks and operational inefficiencies.