Billing & Revenue Cycle Solutions for
Behavioral Health
At UnisLink, we understand the complexities and nuances of behavioral health medical billing. Your focus is on providing essential care to your patients, not on navigating the intricate world of claims and denials. Our specialized Revenue Cycle Management (RCM) solutions are designed to address the unique challenges behavioral health practices face, ensuring you maximize revenue and can concentrate on what matters most—your patients.
Read our blog article
A Comprehensive Look at Medical Coding for Behavioral Health Specialties
UnisLink – Tailored Specifically for Behavioral Health Groups
Overcoming Common Behavioral Health Billing Pain Points
Many behavioral health providers struggle with issues that are specific to the specialty. Our behavioral health billing services are built to solve these key challenges.
- Low Reimbursement & Complex Payer Rules – Most behavioral heal providers face low reimbursement rates and ever-changing payer policies, especially with commercial and government payers. UnisLink’s expert medical billers and coders are specialists in behavioral health. We stay up-to-date on all the latest requirements, updates, coding rules codes (like those for teletherapy and group sessions), policies, and regulations to ensure claims are accurate and maximize your reimbursement.
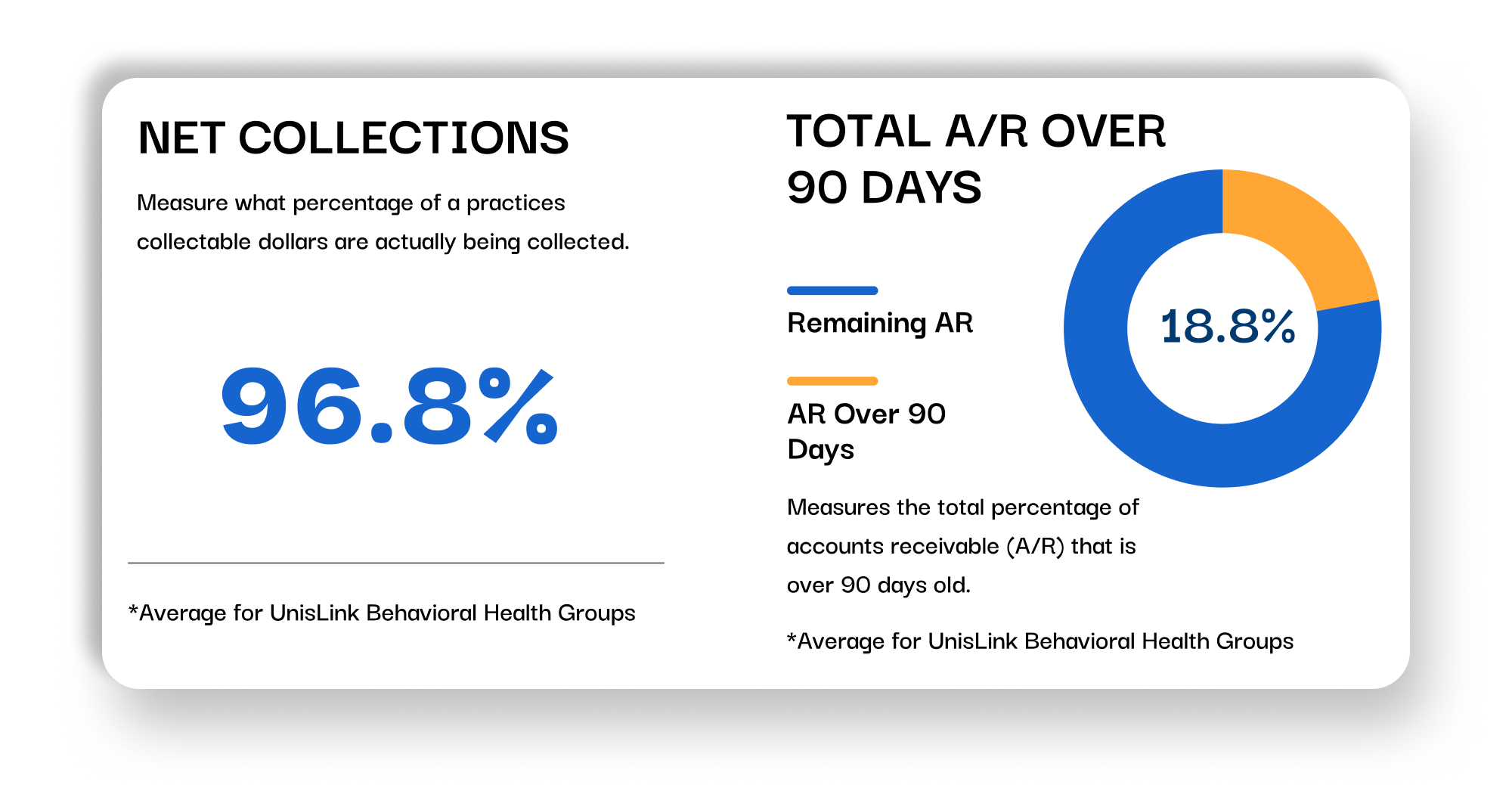
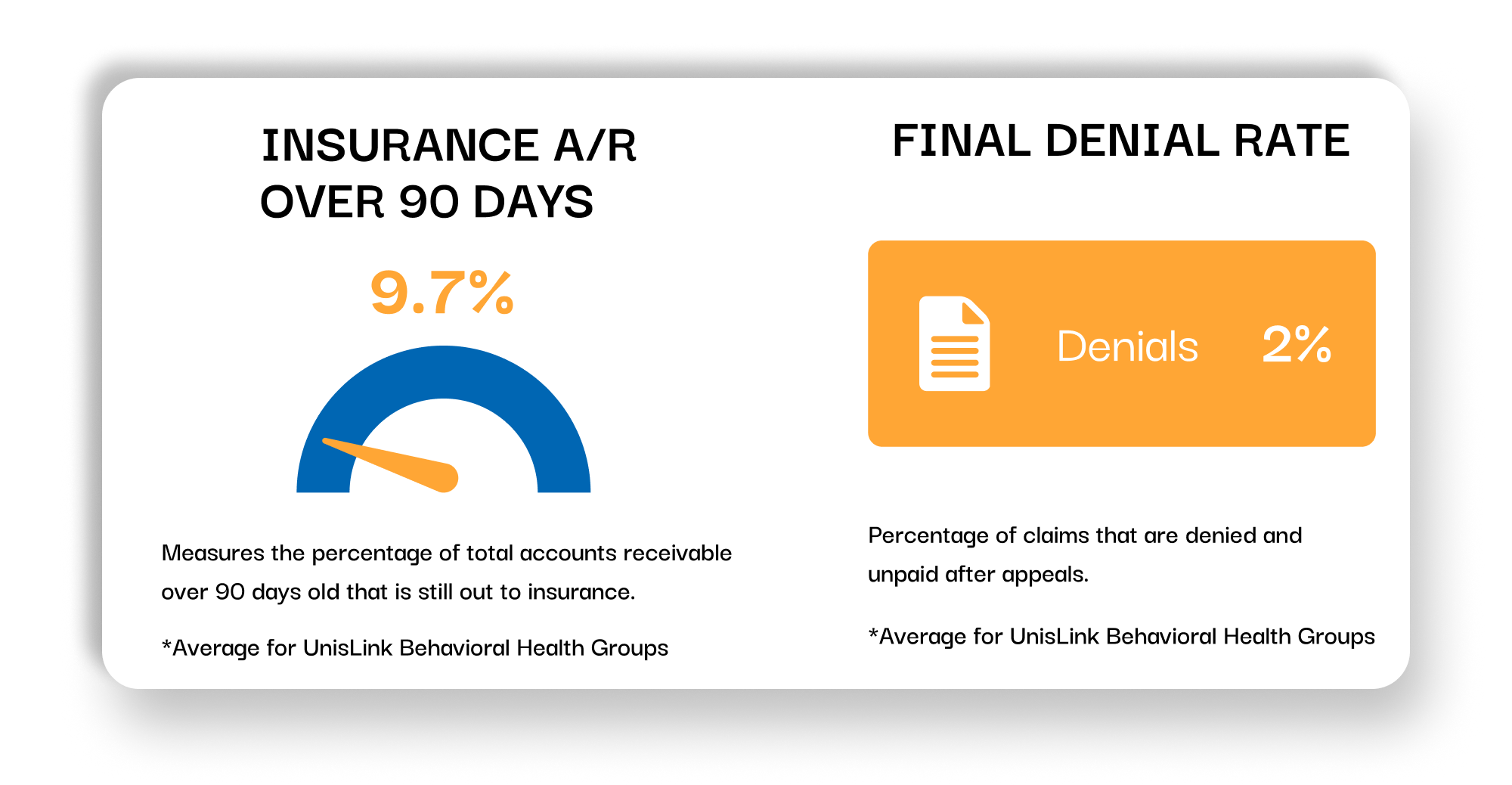
- Claim Denials & Unpaid A/R – Inconsistent documentation, incorrect CPT codes, and missed authorization requirements can lead to high denial rates and a backlog of unpaid claims. UnisLink provides comprehensive technology for managing the claims scrubbing and submission of claims, catching errors before they become denials. Our dedicated AI-enabled follow-up team diligently work to manage your accounts receivable and appeal denied claims to ensure you get paid for the services you provide.
- Patient Collections – The sensitive nature of behavioral health can make patient collections difficult, leading to a significant portion of your revenue being left on the table. Our AI-driven patient collections process is automated and compassionate making it easy for patients to pay, improving your revenue and reducing the administrative burden on your staff. Frequency and communication channel (text, email, paper statement or phone) are determined uniquely for every patient to maximize propensity to pay while dramatically lowering the cost to collect from patients.
- Credentialing & Enrollment – Getting credentialed with insurance networks is a time-consuming and frustrating process that can delay your ability to see patients and get paid. Using special software UnisLink streamlines the entire credentialing process for you. Our team manages all paperwork, submissions, and follow-ups, ensuring you are enrolled with payers quickly and accurately, and your revenue stream is uninterrupted.
- Technology Adoption – Technology moves quickly and it’s challenging to evaluate (let alone adopt) the best solutions for your practice. UnisLink’s proprietary Artificial Intelligence (AI), Analytics, and SmartHub Workflow systems augment and deliver the best financial performance regardless of the platform you’re using.
- Integration With Your EHR – We add important technological enhancements while working directly within your existing EHR to capture every billable service and streamline your workflow, from check-in to final payment.
Total Transparency: With our Engage Analytics™ platform, you get real-time, transparent access to your practice’s financial health, giving you the insights you need to make smart, data-driven decisions.
Why Partner with UnisLink for Your Behavioral Health Billing?
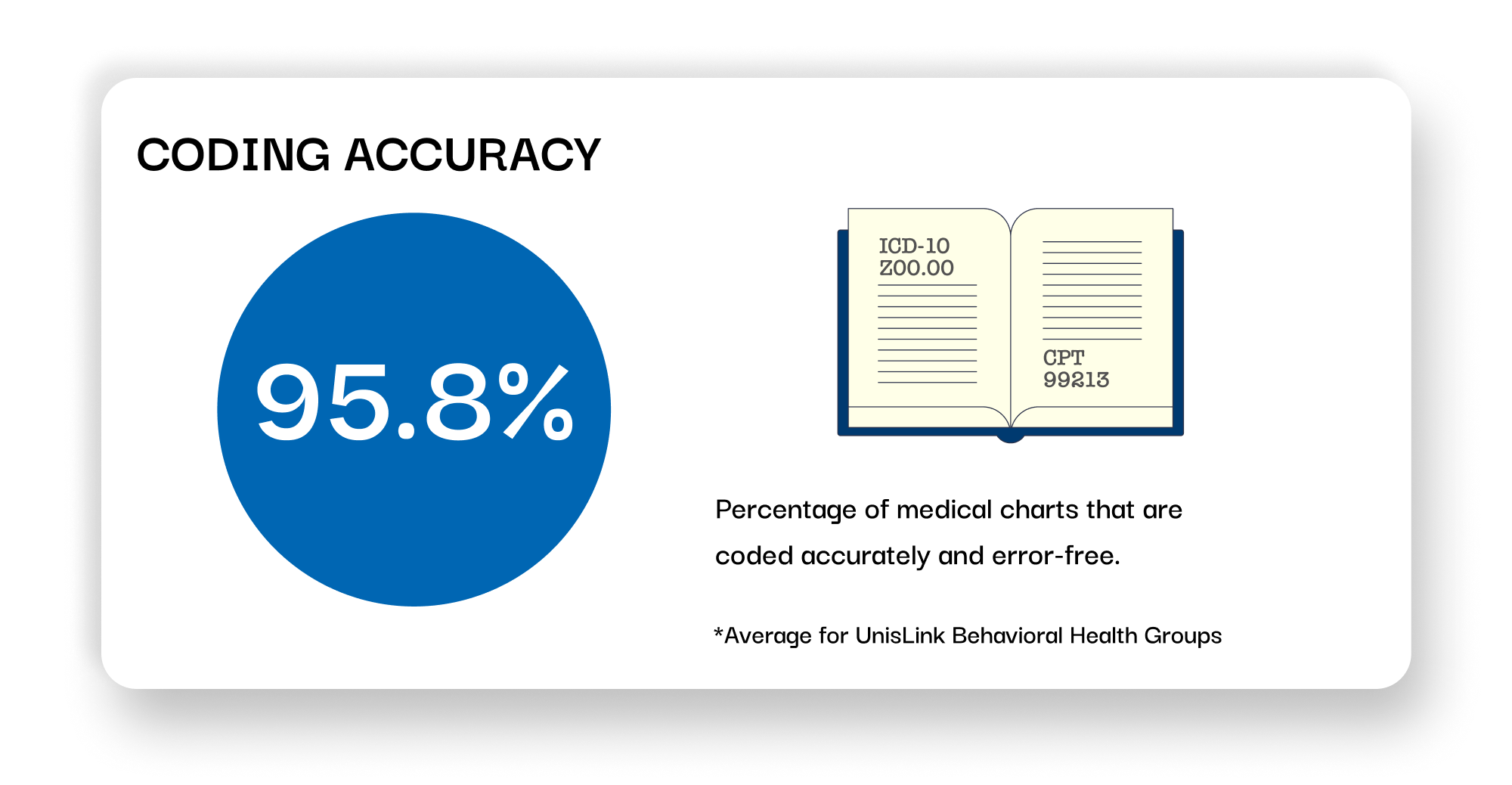
- Behavioral Health Expertise: Our team possesses in-depth knowledge of behavioral health codes and payer requirements.
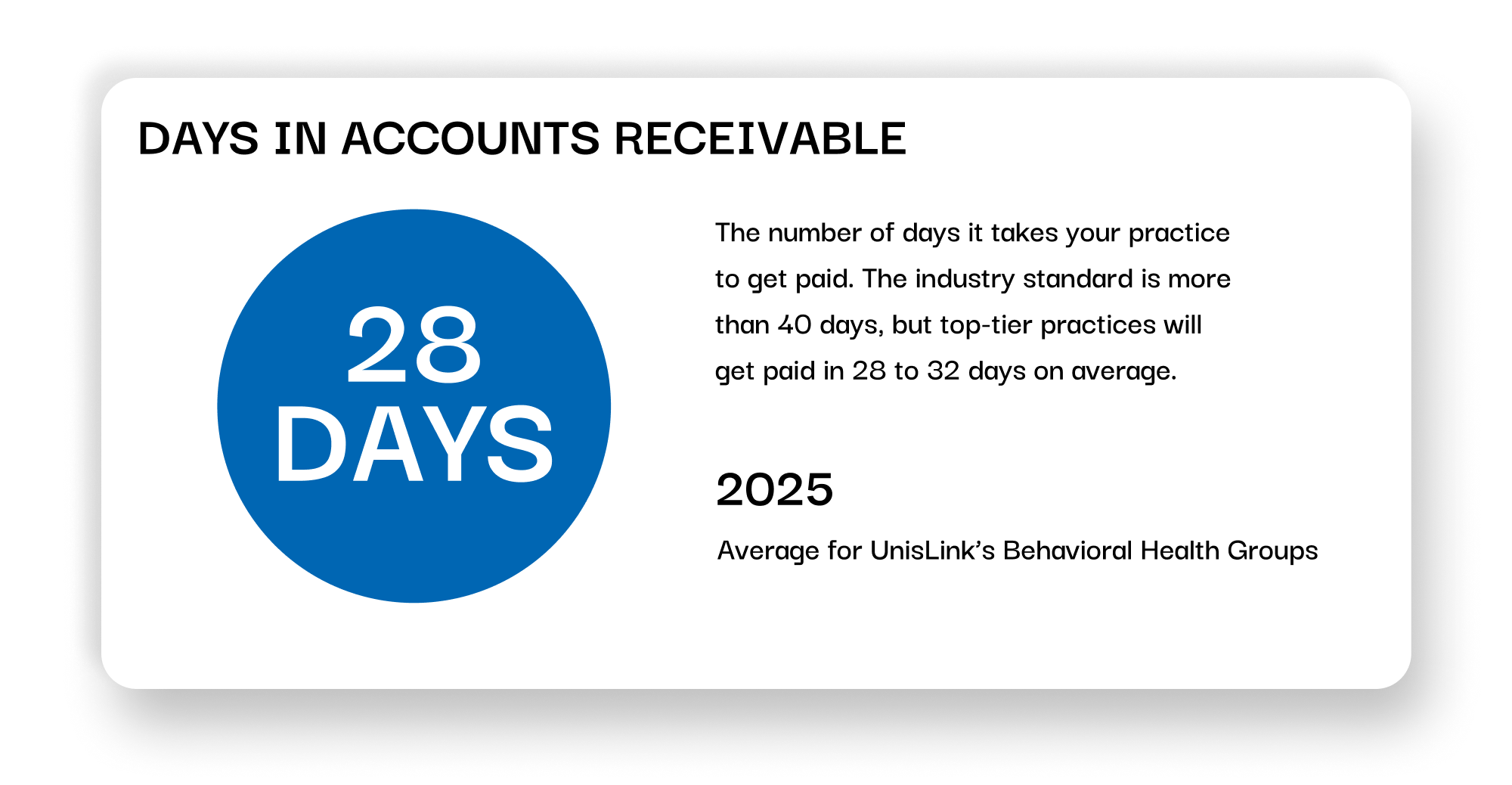
- Faster, More Accurate Payments: Our services are designed to increase first-pass claim acceptance rates and accelerate your cash flow.
- Reduced Administrative Burden: We take the administrative work off your plate, allowing you to focus on clinical excellence.
- Full Transparency: Our advanced reporting and analytics platform, Engage™, gives you real-time visibility into your practice’s financial health, offering actionable insights to improve performance.
Whether you’re a solo practitioner or a multi-location group, UnisLink has the experience and technology to enhance your practice’s profitability. Let us handle the complexities of your revenue cycle so you can get back to providing the compassionate care your patients deserve.
Ready to see how our medical billing services can help your practice thrive?
UnisLink empowers behavioral health groups with a comprehensive, single-source Revenue Cycle Management (RCM) solution, designed to streamline your billing processes and maximize revenue. Our expert team handles every aspect of the revenue cycle, from charge capture and coding to claims submission and payment posting. We stay ahead of evolving payer regulations and quality measures, ensuring your practice remains compliant and receives maximum reimbursement. With UnisLink, you can focus on what matters most: providing exceptional patient care.
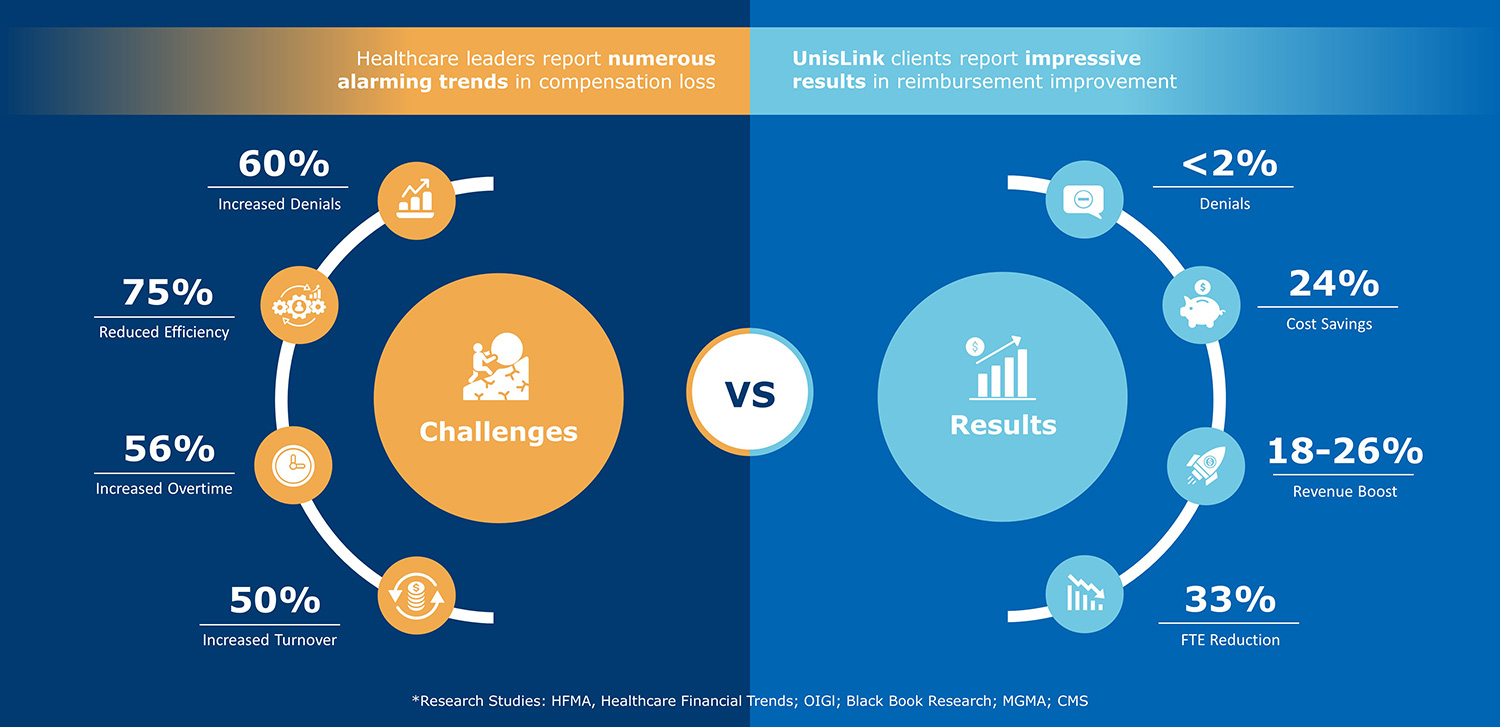
How much revenue improvement can you expect?
Improve your claim submission accuracy and increase cash flow by uncovering leaks and operational inefficiencies.